Overview

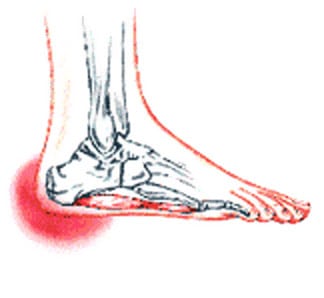
Heel pain is a common foot condition. It's usually felt as an intense pain when using the affected heel. Heel pain usually builds up gradually and gets worse over time. The pain is often severe and occurs when you place weight on the heel. In most cases, only one heel is affected, although estimates suggest that around a third of people have pain in both heels. The pain is usually worse first thing in the morning, or when you first take a step after a period of inactivity. Walking usually improves the pain, but it often gets worse again after walking or standing for a long time. Some people may limp or develop an abnormal walking style as they try to avoid placing weight on the affected heel.
Causes
There is no one cause of heel pain. Whole text books have been written on Disorders of the Heel. Some of the types of problems that can be seen in the heel include Heel spurs, these are small bony spurs that often develop on the bottom of the heel. They do not really cause any problems. It is only mentioned here as it is a common myth that they are a problem - almost always the pain associated with heel spurs is really plantar fasciitis. Plantar fasciitis is the most common cause of heel pain and is due to a strain of the long ligament along the bottom of the foot. The most symptom is pain when getting out of bed first thing in the morning ('post-static dyskinesia') A number of disease processes can uncommonly cause heel pain, such as rheumatoid arthritis, ankylosing spondylitis and gout. Stress fractures, which is an abnormal reaction of bone to stress can occur in those that are very active (eg athletes) or have weaker bones (eg osteoporosis) Pain at the back of the heel could be due to a number of problems, there could be a bursitis at the back of the heel bone (sometimes called 'Haglund's) there could be problems with the insertion of the achilles tendon, such as tendonitis or calcification. A 'stone' bruise is sometimes considered to be a cause of heel pain, its is simply a bruise of the bone. Another cause of heel pain is problems in the calf muscles that refer pain to the heel (myofascial trigger points) or pain referred from the lower back via the nerves from the back to the heel. Heel pain in children is usually due to severs disease or calcaneal apophysitis.
Symptoms
The primary symptom is pain in the heel area that varies in severity and location. The pain is commonly intense when getting out of bed or a chair. The pain often lessens when walking.
Diagnosis
A biomechanical exam by your podiatrist will help reveal these abnormalities and in turn resolve the cause of plantar fasciitis. By addressing this cause, the patient can be offered a podiatric long-term solution to his problem.
Non Surgical Treatment
Physical medicine modalities are well known for their benefits and they have been consistently applied in early treatment of plantar fasciitis. Typically, the direct application of ice, ice baths or contrast soaking aid in the local reduction of inflammation and temporarily augment pain management. Electric stimulation may only provide indirect reduction of interstitial inflammation of the plantar fascia. Ultrasound therapy, hot pack systems and deep tissue massage help eliminate inflammation and aid in restoring plantar fascia tensegrity. Generally, these modalities are considered to be valuable adjuncts to a well-organised treatment plan. Various programs of stretching, range of motion and therapeutic exercises can help re-establish foot function and improve tolerance to load. When it is done appropriately, stretching can serve as an important adjunct to the resumption of the plantar fascia?s ability to tolerate eccentric loading forces that typically occur during stance and gait. Night splinting has proven to be an effective tool in managing persistent plantar fasciitis. Antiinflammatory modalities, such as ice and ice baths, are often the first line of treatment. Oral NSAIDs have been a mainstay of treatment. While they effectively relieve symptoms, be aware that they frequently fail to promote sustained relief. When inflammation is severe or fails to respond to initial efforts, one may consider corticosteroid injection(s). However, keep in mind that corticosteroid injections impose the risk of aponeurosis rupture secondary to focal collagen tissue necrosis and can result in focal heel fat pad atrophy.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
no foot pain
Prevention
Being overweight can place excess pressure and strain on your feet, particularly on your heels. Losing weight, and maintaining a healthy weight by combining regular exercise with a healthy, balanced diet, can be beneficial for your feet. Wearing appropriate footwear is also important. Ideally, you should wear shoes with a low to moderate heel that supports and cushions your arches and heels. Avoid wearing shoes with no heels.

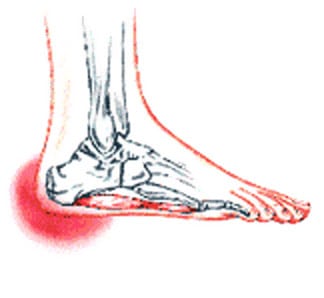
Heel pain is a common foot condition. It's usually felt as an intense pain when using the affected heel. Heel pain usually builds up gradually and gets worse over time. The pain is often severe and occurs when you place weight on the heel. In most cases, only one heel is affected, although estimates suggest that around a third of people have pain in both heels. The pain is usually worse first thing in the morning, or when you first take a step after a period of inactivity. Walking usually improves the pain, but it often gets worse again after walking or standing for a long time. Some people may limp or develop an abnormal walking style as they try to avoid placing weight on the affected heel.
Causes
There is no one cause of heel pain. Whole text books have been written on Disorders of the Heel. Some of the types of problems that can be seen in the heel include Heel spurs, these are small bony spurs that often develop on the bottom of the heel. They do not really cause any problems. It is only mentioned here as it is a common myth that they are a problem - almost always the pain associated with heel spurs is really plantar fasciitis. Plantar fasciitis is the most common cause of heel pain and is due to a strain of the long ligament along the bottom of the foot. The most symptom is pain when getting out of bed first thing in the morning ('post-static dyskinesia') A number of disease processes can uncommonly cause heel pain, such as rheumatoid arthritis, ankylosing spondylitis and gout. Stress fractures, which is an abnormal reaction of bone to stress can occur in those that are very active (eg athletes) or have weaker bones (eg osteoporosis) Pain at the back of the heel could be due to a number of problems, there could be a bursitis at the back of the heel bone (sometimes called 'Haglund's) there could be problems with the insertion of the achilles tendon, such as tendonitis or calcification. A 'stone' bruise is sometimes considered to be a cause of heel pain, its is simply a bruise of the bone. Another cause of heel pain is problems in the calf muscles that refer pain to the heel (myofascial trigger points) or pain referred from the lower back via the nerves from the back to the heel. Heel pain in children is usually due to severs disease or calcaneal apophysitis.
Symptoms
The primary symptom is pain in the heel area that varies in severity and location. The pain is commonly intense when getting out of bed or a chair. The pain often lessens when walking.
Diagnosis
A biomechanical exam by your podiatrist will help reveal these abnormalities and in turn resolve the cause of plantar fasciitis. By addressing this cause, the patient can be offered a podiatric long-term solution to his problem.
Non Surgical Treatment
Physical medicine modalities are well known for their benefits and they have been consistently applied in early treatment of plantar fasciitis. Typically, the direct application of ice, ice baths or contrast soaking aid in the local reduction of inflammation and temporarily augment pain management. Electric stimulation may only provide indirect reduction of interstitial inflammation of the plantar fascia. Ultrasound therapy, hot pack systems and deep tissue massage help eliminate inflammation and aid in restoring plantar fascia tensegrity. Generally, these modalities are considered to be valuable adjuncts to a well-organised treatment plan. Various programs of stretching, range of motion and therapeutic exercises can help re-establish foot function and improve tolerance to load. When it is done appropriately, stretching can serve as an important adjunct to the resumption of the plantar fascia?s ability to tolerate eccentric loading forces that typically occur during stance and gait. Night splinting has proven to be an effective tool in managing persistent plantar fasciitis. Antiinflammatory modalities, such as ice and ice baths, are often the first line of treatment. Oral NSAIDs have been a mainstay of treatment. While they effectively relieve symptoms, be aware that they frequently fail to promote sustained relief. When inflammation is severe or fails to respond to initial efforts, one may consider corticosteroid injection(s). However, keep in mind that corticosteroid injections impose the risk of aponeurosis rupture secondary to focal collagen tissue necrosis and can result in focal heel fat pad atrophy.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
no foot pain
Prevention
Being overweight can place excess pressure and strain on your feet, particularly on your heels. Losing weight, and maintaining a healthy weight by combining regular exercise with a healthy, balanced diet, can be beneficial for your feet. Wearing appropriate footwear is also important. Ideally, you should wear shoes with a low to moderate heel that supports and cushions your arches and heels. Avoid wearing shoes with no heels.
 RSS Feed
RSS Feed
